
Congestive heart failure (CHF) is a chronic condition where the heart struggles to pump blood efficiently, leading to a variety of health issues. This comprehensive guide will walk you through the stages, symptoms, causes, diagnosis, treatment, pathophysiology, and stages of dying associated with CHF. Whether you’re a patient, caregiver, or just someone looking to understand more about this condition, this article will provide valuable insights.
What are the 4 Stages of Congestive Heart Failure?
Congestive heart failure is classified into four stages, ranging from high risk of developing heart failure to advanced heart failure:
Stage A: High Risk of Developing Heart Failure
Description:
Individuals have risk factors such as hypertension, diabetes, obesity, or a family history of cardiomyopathy. No symptoms or structural heart disease are present.
Management:
Lifestyle changes (diet, exercise), managing underlying conditions, and medications like ACE inhibitors or ARBs.
Stage B: Asymptomatic Heart Failure
Description:
Structural heart disease (e.g., left ventricular dysfunction) is present, but there are no symptoms of heart failure.
Management:
Medications (beta-blockers, ACE inhibitors), lifestyle changes, and regular monitoring.
Stage C: Symptomatic Heart Failure
Description:
Patients exhibit symptoms of heart failure associated with structural heart disease.
Management: Medications (diuretics, aldosterone antagonists), lifestyle modifications, and possibly devices like implantable cardioverter-defibrillators (ICDs).
Stage D: Advanced Heart Failure
Description:
Noticeable heart failure signs even at rest even with the best possible medical care.
Management:
Advanced treatments such as heart transplant, ventricular assist devices (VADs), or palliative care.

Congestive Heart Failure Symptoms
The symptoms of congestive heart failure can vary depending on the stage and severity of the condition but commonly include:
- Shortness of breath (dyspnea)
- Persistent coughing or wheezing
- Swelling (edema) in the legs, ankles, and feet
- Fatigue and weakness
- Rapid or irregular heartbeat
- Reduced ability to exercise
- Increased need to urinate at night
- Swelling of the abdomen (ascites)
- Sudden weight gain from fluid retention
- Lack of appetite and nausea
- Difficulty concentrating or decreased alertness
Congestive Heart Failure Causes
Congestive heart failure can result from a number of causes, including:
Coronary Artery Disease:
Narrowed arteries reduce blood flow to the heart.
High Blood Pressure (Hypertension):
Causes the heart to work harder than normal.
Cardiomyopathy:
Disease of the heart muscle itself.
Heart Attack:
Damages the heart muscle, affecting its ability to pump efficiently.
Valvular Heart Disease:
Malfunctioning heart valves can strain the heart.
Congenital Heart Defects:
Structural problems present at birth.
Arrhythmias:
Heart failure may result from irregular heart beats.

Congestive Heart Failure Diagnosis
Diagnosing congestive heart failure involves a combination of medical history, physical examination, and diagnostic tests:
Medical History and Physical Exam:
Assessment of symptoms and risk factors.
Blood Tests:
Checking for biomarkers like B-type natriuretic peptide (BNP).
Chest X-ray:
Identifies fluid in the lungs or an enlarged heart.
Electrocardiogram (ECG):
Detects heart rhythm problems.
Echocardiogram:
Uses sound waves to produce images of the heart’s size, structure, and motion.
Stress Tests:
Evaluate the heart’s function during physical activity.
Cardiac MRI:
Gives precise illustrations of the composition and operation of the heart.
Coronary Angiogram:
Checks for blockages in the coronary arteries.
Congestive Heart Failure Treatment
The goals of treatment are to reduce symptoms, enhance quality of life, and delay the course of the illness:
Medications:
Diuretics, ACE inhibitors, beta-blockers, aldosterone antagonists, and more.
Lifestyle Changes:
Low-sodium diet, regular exercise, weight management, quitting smoking, and reducing alcohol intake.
Medical Devices and Surgery:
ICDs, cardiac resynchronization therapy (CRT), VADs, and heart transplant.
Monitoring and Regular Check-ups:
Continuous medical monitoring to modify treatment as necessary.
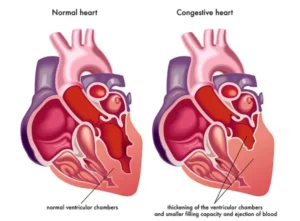
Congestive Heart Failure Pathophysiology
Understanding the pathophysiology of CHF helps explain how the disease progresses:
Heart Muscle Damage:
Caused by conditions like coronary artery disease or hypertension.
Decreased Cardiac Output:
The heart’s inability to pump enough blood to meet the body’s needs.
Neurohormonal Activation:
The body’s compensatory mechanisms, such as activation of the renin-angiotensin-aldosterone system (RAAS), initially help but eventually worsen heart function.
Fluid Retention:
Resulting from hormonal imbalances, leading to symptoms like edema and shortness of breath.
Congestive Heart Failure Stages of Dying
In the final stages of CHF, the focus often shifts to comfort and quality of life:
Increased Symptom Severity:
Worsening shortness of breath, fatigue, and fluid retention.
Frequent Hospitalizations:
Due to exacerbations of heart failure symptoms.
Palliative Care:
Controlling symptoms and offering spiritual, social, and psychological assistance.
Hospice Care:
For those in the last months of life, focusing on comfort rather than curative treatment.
End-of-Life Planning:
Discussing and documenting care preferences with family and healthcare providers.
