
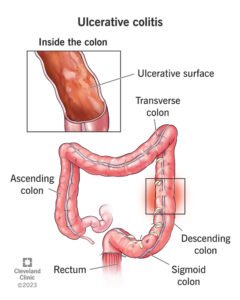
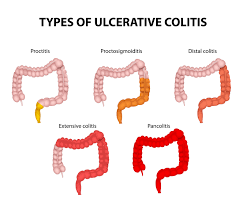
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum, causing inflammation and ulcers. This blog provides a comprehensive overview of UC, including its symptoms, diagnosis, treatments, dietary recommendations, and more.
Ulcerative Colitis Symptoms
Ulcerative colitis symptoms can vary in severity and may develop gradually or suddenly. Common symptoms include:
Abdominal Pain and Cramping:
Often located in the lower left abdomen.
Diarrhea:
Frequently accompanied by blood or pus.
Urgency to Defecate:
Sometimes with an inability to defecate despite the urge.
Weight Loss:
Due to decreased appetite and malabsorption.
Fatigue:
Often related to anemia and overall inflammation.
Fever:
In cases of severe inflammation.
Rectal Pain and Bleeding:
Commonly experienced during bowel movements.
Ulcerative Colitis Symptoms in Females
While both men and women can experience the same general symptoms, some symptoms may be more pronounced in females:
Increased Menstrual Symptoms:
Flare-ups may coincide with menstrual cycles, causing increased pain and gastrointestinal discomfort.
Higher Risk of Anemia:
Due to blood loss during menstruation combined with rectal bleeding.
Bone Density Loss:
Women are generally at a higher risk, especially if taking corticosteroids for long-term treatment.
Ulcerative Colitis Diagnosis
Diagnosing ulcerative colitis involves a series of tests and examinations:
Medical History and Physical Exam:
Initial assessment of symptoms and health history.
Blood Tests:
To look for indicators of infection and anaemia.
Stool Sample:
To rule out infections and detect inflammation markers.
Colonoscopy:
A key diagnostic tool that allows direct visualization and biopsy of the colon.
Flexible Sigmoidoscopy:
Examines the lower part of the colon if a full colonoscopy is not required.
Imaging Tests:
Such as X-rays, CT scans, or MRI to get a detailed view of the colon.

Ulcerative Colitis Treatments
Treatment for ulcerative colitis aims to reduce inflammation, manage symptoms, and maintain remission:
Medications:
Various types are used to treat UC, including aminosalicylates, corticosteroids, immunomodulators, and biologics.
Biologics:
Reducing inflammation in the immune system requires targeting particular pathways.
Janus Kinase (JAK) Inhibitors:
Newer medications that block specific enzymes involved in the inflammatory process.
Antibiotics:
Sometimes used to treat infections that may accompany UC.
What is the Latest Treatment for Ulcerative Colitis?
Recent advancements in UC treatment include:
Biologic Therapies:
Newer biologics like ustekinumab and tofacitinib have shown promise in managing moderate to severe UC.
Fecal Microbiota Transplantation (FMT):
Emerging as a potential therapy to restore healthy gut bacteria balance.
Sphingosine 1-Phosphate (S1P) Receptor Modulators:
Such as ozanimod, showing efficacy in reducing inflammation.
Ulcerative Colitis Surgery
Surgery may be necessary for those who do not respond to medical treatments:
Proctocolectomy with Ileostomy:
Removal of the colon and rectum, with an external pouch to collect waste.
Ileoanal Pouch Anastomosis (J-pouch):
Creating an internal pouch from the end of the small intestine, which is attached to the anus, allowing for normal defecation.
Ulcerative Colitis Medication
Medications for UC include:
Aminosalicylates (5-ASA): Such as mesalamine, to reduce inflammation.
Corticosteroids: For short-term use during flare-ups.
Immunomodulators: Such as azathioprine and methotrexate, to suppress the immune system.
Biologics: Including infliximab and adalimumab, to target specific components of the immune response.
JAK Inhibitors: Like tofacitinib, for patients with moderate to severe UC.
Ulcerative Colitis Diet
Diet plays a crucial role in managing UC symptoms:
Low-Residue Diet:
Reduces the amount of undigested food passing through the colon, easing symptoms during flare-ups.
Anti-Inflammatory Diet:
Focuses on foods that reduce inflammation, such as fatty fish, leafy greens, and nuts.
Hydration:
Ensuring adequate fluid intake is vital, especially during diarrhea episodes.
Avoid Trigger Foods:
Common triggers include dairy, spicy foods, alcohol, and caffeine.
